Fever after iron injection is a potential reaction that occurs during or shortly after intravenous iron therapy. While not always the primary symptom highlighted in medical literature, fever often accompanies other systemic symptoms that healthcare providers classify as infusion reactions or acute hypersensitivity responses. Understanding these reactions—from mild, self-limiting symptoms to rare serious events—is critical for anyone receiving iron replacement therapy.
Intravenous iron has become essential for treating iron deficiency anemia, especially for patients with chronic kidney disease, inflammatory conditions, or gastrointestinal disorders that prevent effective oral iron absorption. The therapy offers significant advantages in bioavailability and speed of repletion. However, like all parenteral treatments, it carries potential risks that require proper understanding and management.
This guide provides specific information about fever following iron injection, including why it happens, how to recognize different reaction types, when to seek immediate help, and what steps you can take to prevent or minimize adverse effects. Whether you’re preparing for your first iron infusion or experiencing symptoms after treatment, this resource will help you respond appropriately.
Identify Iron Infusion Reaction Warning Signs
Fever after iron injection typically appears alongside other symptoms that signal an infusion reaction. Recognizing these early warning signs allows for prompt intervention and prevents complications. Cutaneous symptoms often appear first and include flushing, itching, and hives—these provide crucial early indicators of a developing reaction.
Respiratory symptoms can range from mild chest tightness to significant breathing difficulties, while cardiovascular manifestations may include blood pressure changes, rapid heartbeat, or chest discomfort. General symptoms frequently include anxiety, a sense of impending doom, and temperature dysregulation. If you experience fever along with any of these symptoms during or shortly after your iron infusion, notify medical staff immediately.
Healthcare professionals now understand that most adverse events following intravenous iron result from complement activation-related pseudo-allergy (CARPA), not true IgE-mediated allergic reactions. This distinction matters because it affects how reactions are prevented, recognized, and managed. The nanoparticle nature of iron preparations triggers complement system activation, generating inflammatory mediators that produce symptoms without involving classical allergic pathways.
Minor reactions typically include mild chest and back pressure sensations, flushing, and itching without hypotension, rapid breathing, wheezing, or cardiovascular compromise. These reactions generally resolve spontaneously within 5 to 10 minutes without intervention. While fever isn’t always a defining characteristic of minor reactions, patients may experience warmth sensations or mild temperature elevation during these events.
Why Fever Develops After Iron Injection
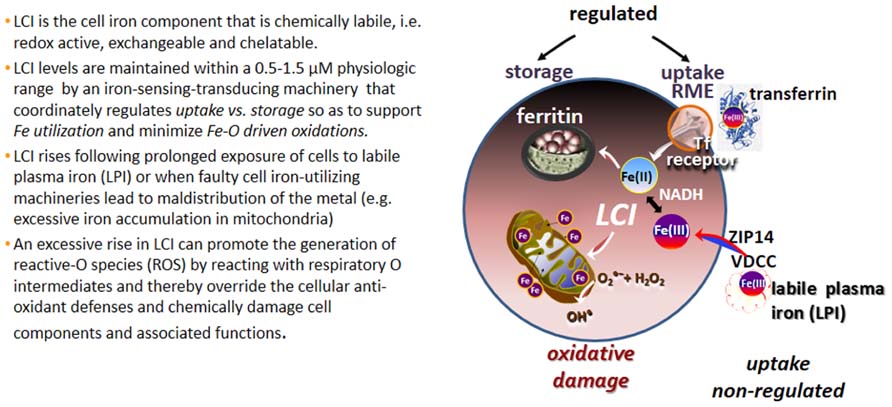
Fever following iron injection primarily results from the physicochemical properties of iron formulations interacting with your body’s immune systems. The underlying mechanism involves the release of labile iron—iron not tightly bound to its carbohydrate shell—when intravenous iron preparations enter your bloodstream.
When labile iron dissociates, it interacts with biological systems in ways that trigger systemic symptoms including temperature dysregulation. Modern formulations with more stable carbohydrate-iron complexes demonstrate improved tolerability because they minimize labile iron release. The more stable the iron preparation, the less likely you are to experience fever or other systemic reactions.
Complement activation-related pseudo-allergy (CARPA) represents the most common pathogenic mechanism behind acute hypersensitivity reactions to current intravenous iron formulations. Unlike true allergies, CARPA occurs when nanoparticle iron preparations activate your complement system, generating anaphylatoxins that trigger mast cell and basophil activation. The resulting release of histamine, thromboxanes, leukotrienes, and platelet-activating factor produces symptoms that may include fever.
Research shows that platelet-activating factor levels correlate with reaction severity: elevated PAF appears in 20% of grade 1 reactions, 66.7% of grade 2 reactions, and 100% of grade 3 reactions. This explains why some patients experience only mild symptoms while others have pronounced reactions to the same iron formulation.
Differentiate Between Reaction Severity Levels

Understanding the different categories of reactions helps you and your healthcare providers respond appropriately to symptoms and make informed decisions about future iron therapy. Reactions range from minor, self-limiting events to rare medical emergencies requiring immediate intervention.
Minor Reactions: What to Expect and How to Respond
Minor infusion reactions represent the most common type of adverse event associated with intravenous iron administration. These reactions typically include chest and back pressure sensations, flushing, itching, and hives but notably without hypotension, rapid breathing, rapid heart rate, wheezing, stridor, or periorbital swelling.
Key characteristics of minor reactions:
– Symptoms usually resolve spontaneously within 5 to 10 minutes
– Rarely progress to serious complications
– Often don’t recur when infusion restarts at a slower rate
– May include sensations of warmth or mild temperature elevation
If you experience these symptoms, inform medical staff immediately but understand the outcome is typically favorable. Your healthcare team will likely monitor you closely and may restart the infusion at a slower rate once symptoms subside.
Recognize Complement Activation-Related Pseudo-Allergy (CARPA)
CARPA reactions may include fever alongside other symptoms requiring medical attention. Symptoms typically appear during or shortly after infusion initiation and may include:
- Cutaneous manifestations: rash, flushing, and pruritus
- Respiratory symptoms: dyspnea, wheezing, throat tightness
- Cardiovascular symptoms: hypotension, tachycardia, chest discomfort
- General symptoms: anxiety, sense of impending doom, temperature dysregulation
The severity of CARPA reactions correlates with platelet-activating factor levels in your bloodstream. Unlike true allergies, CARPA reactions can occur during first-time exposure to iron formulations and don’t necessarily preclude future use of alternative iron preparations.
Prevent Iron Infusion Reactions Before They Start
Effective prevention begins with thorough patient assessment before your first infusion. Your healthcare provider should obtain a comprehensive medication history, focusing on prior reactions to iron preparations or other parenteral therapies. A history of multiple drug allergies, asthma, eczema, or mastocytosis warrants additional precautions.
Patient education is critical for prevention. Before your infusion, you should understand:
– That reactions may occur
– Specific symptoms to watch for (itching, flushing, shortness of breath)
– When and how to summon assistance immediately
The facility where you receive intravenous iron must be equipped to manage potential reactions. Staff should be trained in anaphylaxis recognition and management with appropriate medications and resuscitation equipment immediately available.
Crucially, avoid pre-medication with H1 antihistamines like diphenhydramine for all patients. Evidence shows this practice may actually increase perceived reactions, as first-generation antihistamines can cause somnolence, sweating, hypotension, and tachycardia that may be mistakenly attributed to the iron infusion.
Treat Fever and Infusion Reactions Immediately
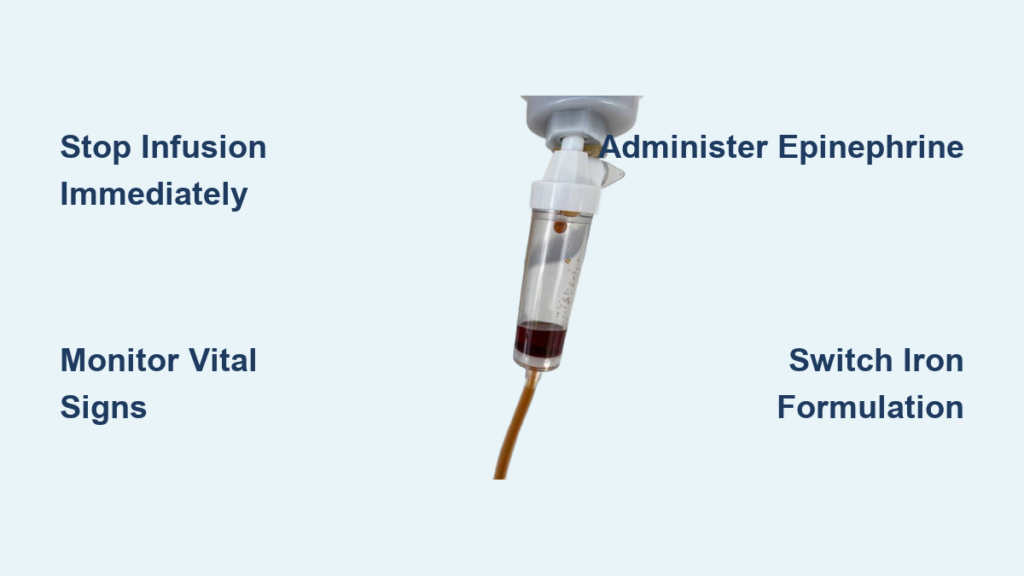
When any adverse reaction occurs during intravenous iron administration, the immediate first step must be cessation of the infusion. Do not wait to confirm the reaction type—stopping the infusion immediately offers the best chance to prevent progression.
Manage Hypotensive Reactions Effectively
If your iron infusion causes low blood pressure:
– Lie down with legs elevated to improve blood flow to your brain
– Receive an intravenous fluid bolus (typically 500 mL of normal saline)
– Have continuous monitoring of heart rhythm, blood pressure, and oxygen levels
While not strongly evidence-based, your healthcare team may administer intravenous corticosteroids and H2 antihistamines during hypotensive reactions. Once stable, they may consider re-challenging with a different iron formulation after evaluating the benefit-risk ratio.
Emergency Response for Anaphylaxis

True anaphylaxis following iron injection is exceedingly rare (less than 1 in 250,000 administrations) but requires immediate, aggressive treatment. Epinephrine is first-line treatment and should be administered as soon as anaphylaxis is suspected without waiting for confirmation.
The recommended epinephrine dose is 0.5 mg of 1:1000 concentration administered intramuscularly into the thigh. This dose may be repeated every 5-15 minutes if no clinical improvement occurs. Supplemental treatments include:
– Intravenous fluids (1,000-2,000 mL of normal saline)
– Nebulized bronchodilators for breathing difficulties
– High-flow oxygen delivery
When to Seek Emergency Medical Help
Call emergency services immediately if you experience any of these symptoms during or after your iron infusion:
– Difficulty breathing or throat swelling
– Sudden drop in blood pressure
– Rapid heartbeat or chest pain
– Loss of consciousness
For symptoms developing after leaving the infusion facility, contact your healthcare provider if:
– Fever exceeds 101°F (38.3°C)
– Symptoms persist or worsen after 24 hours
– You develop severe headache, joint pain, or muscle pain unresponsive to over-the-counter medications
– You notice facial, lip, or tongue swelling
Up to 10% of patients experience delayed arthralgias (joint pains) and myalgias (muscle pains) beginning the day after infusion. While fever isn’t explicitly documented as a common delayed reaction, some patients may experience temperature elevation alongside these symptoms.
Special Considerations for Chronic Conditions
Patients with chronic kidney disease, particularly those on hemodialysis, have extensive experience with intravenous iron therapy. Research shows patients who reacted to one formulation often successfully tolerate others—iron sucrose has been particularly well-tolerated by hemodialysis patients with previous reactions.
For surgical patients, pre-operative anemia significantly increases risks of infection, longer hospital stays, and mortality. Iron deficiency causes most perioperative anemia, making iron repletion essential. Time constraints often favor intravenous over oral iron therapy, as IV iron achieves therapeutic goals more rapidly.
Inflammatory conditions like inflammatory bowel disease or rheumatoid arthritis create functional iron deficiency where oral iron often fails. Modern IV iron formulations show similar safety profiles across these conditions when administered according to protocols.
Long-Term Prevention After Reaction Occurrence
If you’ve experienced fever or other reactions after iron injection, proper follow-up ensures complete symptom resolution. Delayed symptoms like joint and muscle pain may persist for days and might require NSAID treatment.
Document your reaction thoroughly with:
– Specific iron product brand name
– Timing of symptom onset
– Detailed symptoms experienced
– Vital signs during the reaction
– Interventions provided and your response
Future administration of any IV iron formulation is contraindicated only after severe hypersensitivity reactions. For milder reactions, switching to an alternative formulation is often successful. Clinical experience shows patients reacting to one formulation frequently tolerate others without difficulty.
Key Takeaway: Fever after iron injection typically falls within the spectrum of infusion reactions, with modern formulations showing excellent safety profiles (serious events in fewer than 1 in 250,000 administrations). Most reactions result from complement activation-related pseudo-allergy rather than true allergies. Immediate cessation of infusion at first symptoms, proper recognition of reaction severity, and appropriate medical management minimize risks while allowing you to benefit from essential iron repletion therapy. Always discuss reaction history thoroughly with your healthcare provider before future iron treatments.