Feeling constantly exhausted, breathless during routine activities, or noticing unusual paleness can signal your body lacks a fundamental mineral it needs to function. Iron deficiency develops when your iron stores become depleted, leaving insufficient amounts of this essential mineral to produce healthy red blood cells. Without adequate iron, your bloodstream cannot efficiently transport oxygen to tissues throughout your body, creating a cascade of symptoms that gradually worsen if the underlying causes of extremely low iron remain unaddressed.
Iron deficiency represents the most common nutritional disorder globally, affecting people across all demographics. The condition exists on a spectrum, ranging from mildly depleted iron stores with subtle symptoms to severe deficiency that significantly impairs red blood cell production. Understanding why your iron levels drop critically low requires examining four fundamental mechanisms: blood loss that depletes iron faster than replacement, increased physiological demands outpacing intake, inadequate dietary consumption, and impaired absorption preventing utilization of available iron. Most people with severe iron deficiency experience multiple contributing factors rather than a single isolated cause.
Why Hidden Gastrointestinal Bleeding Drains Your Iron Without Warning
Gastrointestinal bleeding stands as the leading cause of iron deficiency in men and post-menopausal women, often progressing silently until severe depletion occurs. The insidious nature of this blood loss means you might experience no obvious blood in stools or changes in bowel habits, making it challenging to detect without medical investigation. Significant iron depletion can develop over months or years from chronic, low-grade bleeding that your body cannot compensate for through dietary absorption alone.
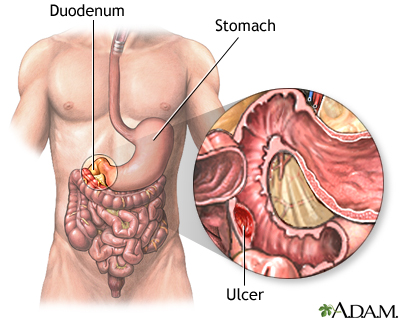
How Stomach Ulcers Trigger Progressive Iron Loss
Stomach ulcers develop when digestive acids erode the stomach lining, creating open sores that bleed slowly over extended periods. While some ulcer-related bleeding causes visible symptoms like vomiting blood or dark stools, many cases produce only hidden blood loss that gradually exhausts your iron reserves. Pro tip: If you take NSAIDs like ibuprofen or aspirin regularly for pain management, you face elevated risk for this iron-depleting complication, as these medications damage your stomach’s protective mechanisms.
Why Bowel Cancer Requires Immediate Investigation
Gastrointestinal cancers, particularly stomach and bowel cancer, sometimes present with iron deficiency anemia as an early warning sign before other symptoms emerge. Adults over age sixty with unexplained iron deficiency anemia require prompt specialist evaluation to rule out underlying malignancy. Medical guidelines mandate urgent referral pathways ensuring appointments within two weeks of initial presentation for this critical diagnostic window.
How Heavy Menstrual Bleeding Causes Rapid Iron Depletion in Women

For women of reproductive age, monthly menstrual periods constitute the most common cause of iron deficiency anemia. The blood lost during each cycle gradually depletes iron stores, with this effect dramatically amplified in women experiencing heavy or prolonged periods. Medically termed menorrhagia, heavy menstrual bleeding involves significant blood loss over multiple consecutive cycles that consistently exceeds your body’s capacity to replace iron through dietary absorption alone.
Visual cue: If you’re soaking through pads or tampons every hour for several hours, needing double protection, or passing large blood clots during your period, you’re likely losing enough iron to cause deficiency. Women with these symptoms should consult a healthcare provider immediately, as untreated heavy bleeding can lead to severe iron depletion within months.
Pregnancy Iron Demands That Outpace Your Body’s Supply
Pregnancy creates one of the most significant increases in iron demand that any individual experiences. Your body must produce substantially more blood to support expanding maternal blood volume, placental development, and your baby’s circulatory system. The growing fetus requires continuous oxygen and nutrient delivery through your blood, making iron absolutely essential for healthy development.
Critical timeline: Without adequate iron intake or supplementation, pregnancy can quickly exhaust maternal iron stores and trigger anemia. Research shows babies born to mothers with untreated anemia face elevated risks of low birth weight and other complications affecting both immediate and long-term health. Most pregnant women require prenatal iron supplements to meet these dramatically increased demands.
The Silent Impact of Vegetarian and Vegan Diets on Iron Levels
Individuals following vegetarian or vegan diets face increased iron deficiency risk because they exclude heme iron sources entirely. Studies consistently demonstrate higher rates of iron deficiency among those following plant-based diets compared to meat consumers. However, obtaining adequate iron through a well-planned vegetarian or vegan diet remains entirely achievable by emphasizing iron-rich plant foods.
Essential Plant-Based Iron Sources You’re Missing
Include these high-iron plant foods in your daily diet to prevent depletion:
– Legumes (lentils, chickpeas, kidney beans)
– Tofu and tempeh
– Nuts and seeds (pumpkin, sesame, hemp)
– Iron-fortified cereals
– Dark leafy greens (spinach, kale)
Expert note: Pair these iron-rich foods with vitamin C sources (citrus fruits, bell peppers, broccoli) to enhance absorption by up to 6 times. Avoid consuming tea, coffee, or calcium supplements within two hours of iron-rich meals, as these inhibit absorption.
Why Bariatric Surgery Patients Face Extreme Iron Loss
Bariatric surgery fundamentally alters your iron absorption capacity by removing or bypassing portions of your stomach and intestines. Gastrectomy reduces stomach acid production necessary for converting dietary iron into absorbable forms, while procedures bypassing the duodenum eliminate the primary site where iron absorption occurs. These surgical changes create a permanent reduction in your body’s ability to absorb dietary iron.
Warning: If you’ve had bariatric surgery, standard iron supplements often prove ineffective. You’ll likely require specialized formulations, higher supplemental doses, or intravenous iron to maintain adequate levels. Regular monitoring of your iron status through blood tests is essential—don’t wait for symptoms to appear before addressing potential deficiency.
Medication Side Effects That Block Iron Absorption Completely

Common medications for acid reflux, heartburn, and ulcer conditions significantly reduce iron absorption by suppressing stomach acid production. Proton pump inhibitors, H2 receptor antagonists, and antacids all interfere with the acidic environment required for optimal iron uptake. If you take these medications regularly, you may unknowingly be sabotaging your body’s ability to absorb dietary iron.
Timing solution: Healthcare providers typically recommend separating these medications from iron supplements by at least two hours before or four hours after taking the acid-reducing medication. Additionally, avoid enteric-coated iron tablets, as their delayed release may bypass your primary iron absorption sites entirely.
Recognizing Critical Iron Deficiency in High-Risk Groups
Identifying individuals at elevated risk enables targeted screening and prevention efforts, ensuring that iron deficiency gets detected before progressing to severe anemia. Women of reproductive age face inherently higher risk due to menstrual blood losses, with this risk intensifying dramatically for those experiencing heavy menstrual bleeding. Infants fed cow’s milk before age one face double jeopardy—minimal iron intake plus microscopic intestinal bleeding that accelerates depletion.
Urgent action required: Frequent blood donors progressively deplete iron stores with each donation. The body requires 24-30 weeks to fully replenish these losses, and regular donors who don’t adjust dietary intake may develop deficiency despite maintaining acceptable hemoglobin levels. If you donate blood regularly, request ferritin testing at your next appointment to assess your actual iron stores.
Critical warning: Left unaddressed, severe iron deficiency progresses to increasingly serious complications affecting multiple body systems. Your cardiovascular system strains to compensate for reduced oxygen-carrying capacity, potentially progressing to heart failure in extreme cases. Immune function becomes compromised, increasing infection susceptibility. Cognitive effects including poor concentration and persistent fatigue significantly impact quality of life.
Understanding the specific causes of extremely low iron in your situation enables targeted intervention that addresses both the immediate deficiency and underlying factors responsible. If you’re experiencing symptoms of iron deficiency, consult your healthcare provider for appropriate testing and treatment—don’t wait until your iron levels reach dangerously low levels before taking action. Early identification and treatment of the root cause can restore your iron status while preventing recurrence and serious complications.





