Waking up with chest discomfort hours after your iron infusion can send your heart racing for all the wrong reasons. If you’ve recently received intravenous iron treatment for iron deficiency anemia and now feel tightness, pressure, or pain in your chest, you’re not alone—this documented side effect affects numerous patients despite iron infusions being generally safe and effective. Understanding why this happens and knowing exactly what to do next can mean the difference between a minor scare and a medical emergency. This guide cuts through the confusion to give you clear, actionable steps for responding to chest pain after iron infusion, helping you distinguish between temporary discomfort and symptoms requiring immediate medical attention.
Iron infusions deliver iron directly into your bloodstream through an IV line, bypassing digestive issues that often prevent patients from tolerating oral supplements. While these treatments typically take just 15-30 minutes and can deliver up to 1,000 milligrams of iron per session, they carry specific risks you must understand. Chest pain ranks among the “more common” side effects documented for iron sucrose injections, meaning healthcare providers routinely monitor for this symptom during and after treatment. Recognizing the potential causes and appropriate responses empowers you to act swiftly and safely if discomfort strikes.
Why Iron Infusion Triggers Chest Discomfort
Iron sucrose injections specifically list chest pain and tightness as “more common” side effects according to prescribing information from medical authorities. Your body may react to the rapid introduction of iron through several mechanisms: sudden blood volume expansion during infusion can create pressure sensations, vasomotor responses may cause blood vessels to constrict or dilate unexpectedly, and positioning during treatment sometimes leads to muscle strain that radiates to the chest area.
The classification as a “more common” side effect doesn’t mean you should ignore it—rather, it indicates healthcare providers expect to monitor for this symptom. Some patients experience referred pain from the IV site that feels like chest discomfort, while others develop true cardiovascular reactions. Understanding these potential causes helps you assess whether your symptoms align with typical infusion reactions or signal something more serious requiring immediate intervention.
Spotting Danger Signs Beyond Normal Discomfort
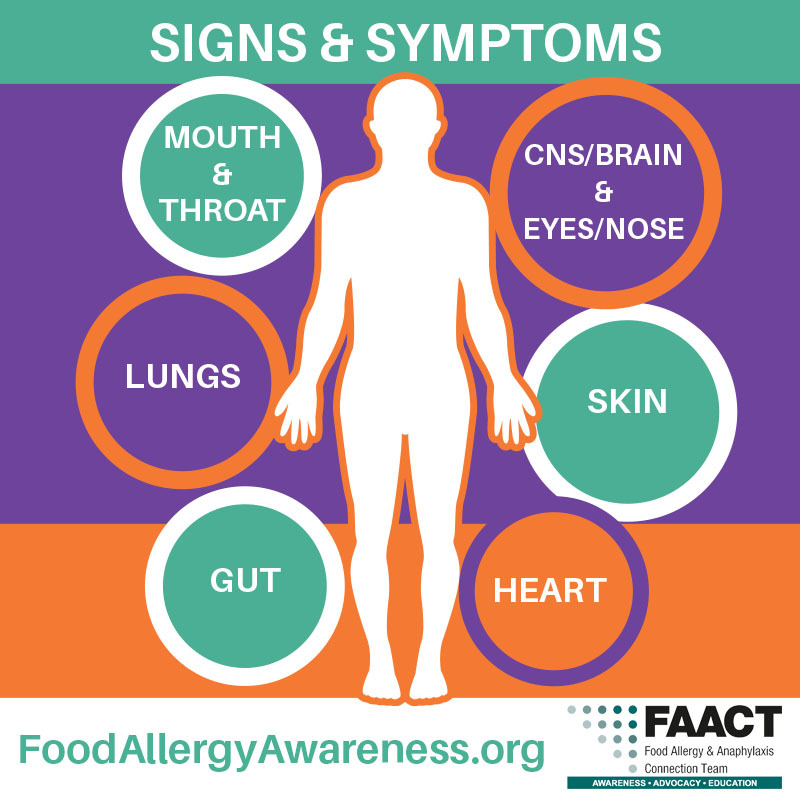
Chest pain after iron infusion becomes an emergency when accompanied by specific warning signs indicating possible anaphylaxis or cardiovascular complications. Contact emergency services immediately if you experience any of these combinations:
- Chest pain with difficulty breathing, wheezing, or shortness of breath
- Tightness in your chest along with facial swelling, tongue swelling, or throat constriction
- Pain radiating to your arm, neck, or jaw accompanied by cold sweats
- Dizziness or lightheadedness that makes standing difficult
- Rapid or irregular heartbeat along with nausea
The first hour after your infusion represents the highest risk period for severe reactions, which is why medical facilities monitor patients for at least 30 minutes post-treatment. However, delayed reactions can occur up to 24 hours later, so remain vigilant even after leaving the clinic. If your chest discomfort persists beyond a few hours or worsens over time, seek medical evaluation regardless of other symptoms.
Critical Actions to Take During Chest Pain Episodes
When chest pain strikes after your iron infusion, follow this immediate action plan:
During the infusion session:
– Press the call button immediately—don’t wait to see if symptoms improve
– Describe your symptoms specifically: “I feel pressure in the center of my chest that’s getting worse”
– Remain seated or lying down until medical staff arrives
After leaving the medical facility:
– Call your healthcare provider immediately—don’t wait until morning
– If symptoms include breathing difficulties or swelling, dial emergency services
– Note the exact time symptoms began and any activities that preceded them
– Have someone drive you to the emergency room if symptoms are moderate
Never attempt to:
– Self-diagnose using internet searches
– Take over-the-counter pain relievers without medical advice
– Drive yourself to the hospital during active chest pain
– Assume symptoms will resolve on their own
If you have a history of severe allergies and carry epinephrine, use it according to your emergency action plan while waiting for help. Even if symptoms improve after using epinephrine, you still require medical evaluation due to potential biphasic reactions.
High-Risk Factors That Increase Complication Chances

Certain conditions significantly elevate your risk for serious reactions during iron infusion. Elderly patients face higher vulnerability due to age-related cardiovascular changes that complicate iron metabolism. If you’re over 65, ensure your provider adjusts monitoring protocols accordingly. Patients with pre-existing heart conditions—including arrhythmias, coronary artery disease, or heart failure—require specialized assessment before infusion.
Hypotension (low blood pressure) creates particular concern as iron sucrose may worsen this condition, sometimes manifesting as chest discomfort. If you regularly experience dizziness when standing or have documented low blood pressure, discuss alternative treatment approaches with your doctor. Iron overload represents an absolute contraindication for additional iron therapy—patients with hemochromatosis or similar conditions should never receive iron infusions.
Your medication history matters too. Disclose all current medications, especially blood pressure drugs, blood thinners, or previous allergy treatments. Any history of medication reactions—particularly to IV medications—warrants thorough discussion before proceeding with iron infusion.
Home Monitoring Protocol for First 48 Hours
After your infusion, implement this monitoring routine at home:
First 24 hours:
– Check blood pressure every 4 hours using a home monitor
– Rate any chest sensations on a 1-10 scale (1=mild, 10=severe)
– Note whether pain changes with position, breathing, or movement
– Keep a symptom journal with exact timing of each episode
Warning signs requiring immediate contact with your provider:
– Blood pressure readings more than 20 points above or below your normal
– Chest discomfort lasting longer than 15 minutes
– Pain that wakes you from sleep
– Symptoms returning after initially subsiding
Most infusion-related side effects resolve within 3-7 days. If your chest pain persists beyond one week or worsens over time, contact your healthcare provider for re-evaluation. Documenting your symptoms helps your medical team determine whether future infusions require modified protocols.
Preventing Recurrence During Future Treatments
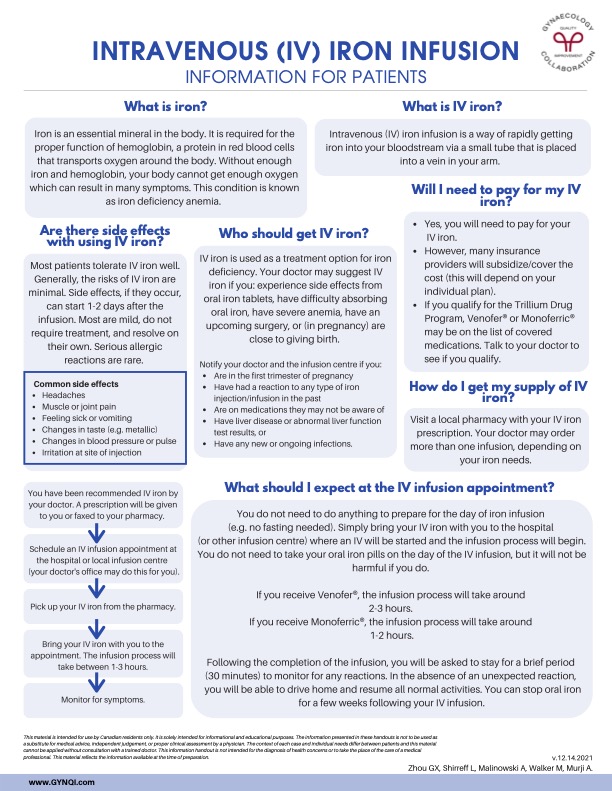
If you experienced chest pain during a previous iron infusion, implement these prevention strategies before your next session:
- Request a slower infusion rate (extend treatment from 15 to 30-60 minutes)
- Ask about pre-medication with antihistamines or corticosteroids
- Choose alternative iron formulations like ferric carboxymaltose if reactions persist
- Schedule infusions during morning hours when your body handles stress better
- Stay well-hydrated before and during treatment to support circulation
Discuss your complete reaction history with your provider before subsequent treatments. Describe exactly when symptoms began (during vs. after infusion), their character (pressure vs. sharp pain), and what relieved them. This information helps your medical team customize your next infusion protocol to minimize recurrence risk while still addressing your iron deficiency.
Managing Persistent Symptoms Without Stopping Treatment
When chest discomfort continues despite preventive measures, these approaches may help you complete necessary iron therapy:
- For muscular discomfort: Apply warm compresses to the chest area and practice gentle stretching
- For mild vasomotor reactions: Try slow, deep breathing exercises during infusion
- For anxiety-related symptoms: Request a quiet treatment room away from medical equipment noise
- For persistent pain: Ask about temporary pain management options compatible with your health status
Your provider may recommend splitting your total iron dose into multiple smaller sessions rather than one large infusion. Some patients benefit from receiving half their dose over two separate appointments spaced a week apart. Always report ongoing symptoms rather than enduring discomfort—your medical team can adjust protocols to maintain treatment effectiveness while improving your comfort.
Recovery Timeline and Long-Term Expectations
Most patients experience complete resolution of infusion-related chest pain within 3-7 days, though full recovery from iron deficiency anemia typically takes up to two months. Don’t assume future infusions will cause identical reactions—many patients successfully receive subsequent treatments with modified protocols. Modern iron formulations prove significantly better tolerated than older versions, with studies showing intravenous iron often works more effectively than oral supplements for appropriate candidates.
If you experienced chest pain during your first infusion, work with your provider to develop a personalized treatment plan for subsequent sessions. This might include slower administration rates, alternative iron compounds, or pre-treatment medications. The overall risk of serious reactions remains low, making iron infusions a valuable option for patients who can’t absorb oral iron. Never avoid necessary treatment due to fear of side effects—instead, partner with your healthcare team to develop the safest possible approach for your specific needs.
Essential Action Steps for Immediate Safety
When chest pain strikes after iron infusion:
– Treat every episode as potentially serious until proven otherwise
– Never drive yourself to the hospital during active chest symptoms
– Keep your healthcare provider’s emergency contact visible at home
– Document symptoms thoroughly for future treatment planning
– Request a detailed reaction report for your medical records
Iron infusions remain a crucial treatment for severe iron deficiency when oral supplements fail, but chest pain requires careful attention. By understanding the warning signs, knowing exactly how to respond, and working with your healthcare team to prevent recurrence, you can safely receive the iron your body needs while minimizing risks. If you experience chest discomfort after your next infusion, follow these protocols and trust your instincts—better to seek evaluation unnecessarily than delay care for a serious reaction.