That persistent fatigue you’re feeling might be more than just a busy schedule—it could signal how low iron affects the body in profound ways. Iron deficiency quietly impacts millions, often starting with subtle signs dismissed as ordinary tiredness. Yet this common nutritional shortfall triggers a chain reaction that compromises your entire oxygen delivery system, affecting everything from your energy levels to your cognitive function. Understanding how low iron affects the body empowers you to recognize symptoms early and seek appropriate care before complications develop.
Without sufficient iron, your body struggles to produce hemoglobin—the essential protein that enables red blood cells to transport oxygen from your lungs to every tissue. This single disruption cascades through multiple body systems, creating symptoms that seem unrelated but share the same root cause. Left unaddressed, iron deficiency can significantly diminish your quality of life, making even routine activities feel exhausting.
This guide reveals exactly how low iron affects the body, helping you identify warning signs and understand when professional evaluation becomes necessary.
Warning Signs of Low Iron
The earliest indicators of iron deficiency often escape notice because they resemble ordinary fatigue or the normal demands of daily life. Your body begins drawing upon stored iron when dietary intake cannot meet daily requirements, and this depletion progressively worsens until symptoms become impossible to ignore. Recognizing these initial warning signs allows for earlier intervention and more effective treatment.
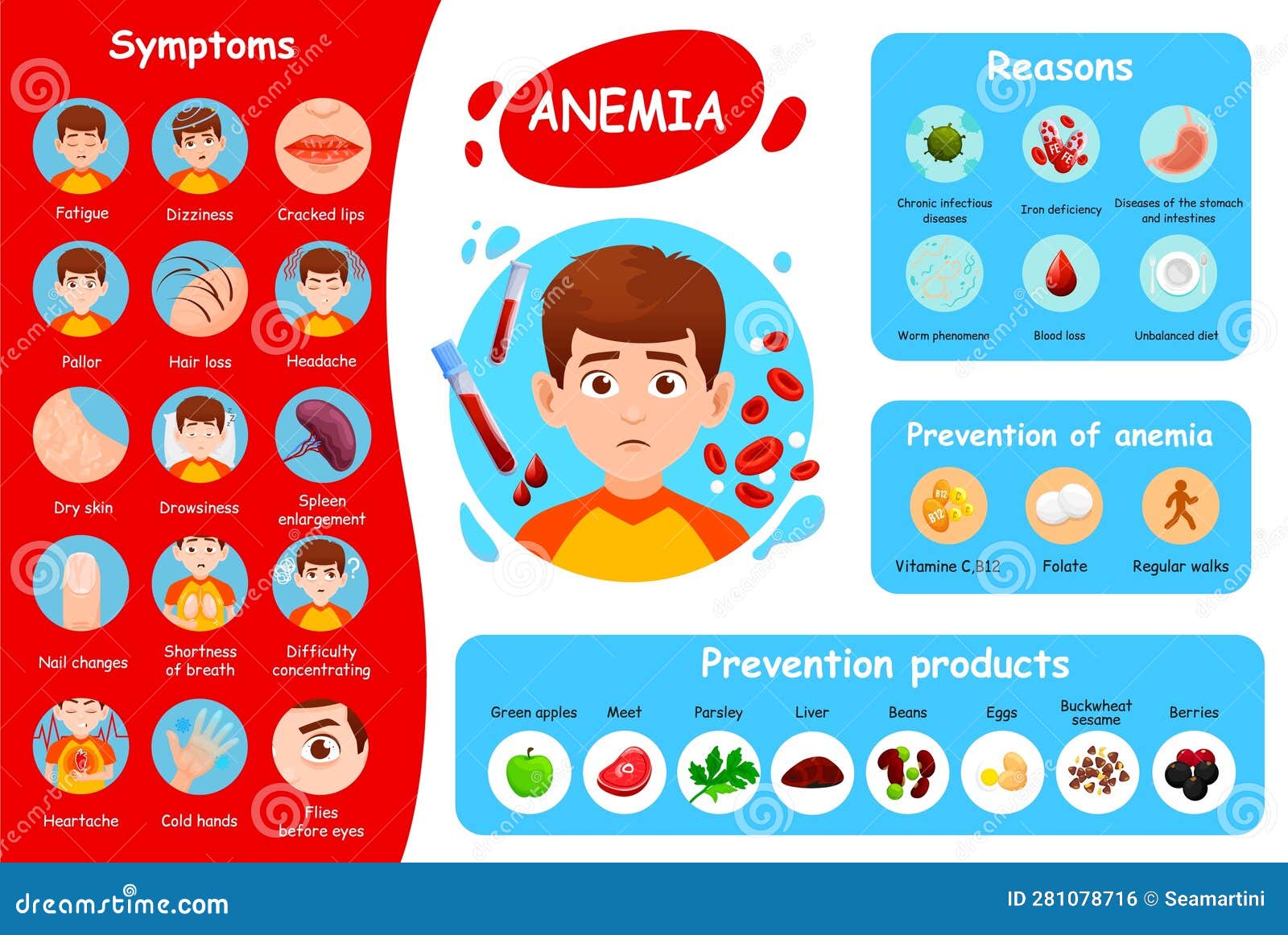
Persistent exhaustion that does not improve with adequate sleep represents one of the first and most common signals of developing deficiency. Unlike normal tiredness that resolves after rest, iron-related fatigue stems from cells receiving inadequate oxygen to produce energy efficiently. You may find yourself needing naps, struggling to complete routine tasks, or feeling drained by midday despite sleeping well the night before.
Unexplained weakness frequently accompanies this fatigue, making activities that previously caused no difficulty feel physically demanding. Your muscles receive less oxygen than they need to function optimally, so climbing stairs, carrying groceries, or even walking at a normal pace may leave you feeling disproportionately tired. This weakness often develops gradually, leading many individuals to attribute it to aging or deconditioning rather than an underlying nutritional deficiency.
Physical Symptoms Explained

As iron deficiency progresses, more visible symptoms emerge that clearly indicate the underlying problem. Understanding these physical manifestations helps you distinguish iron deficiency from other conditions and communicate effectively with healthcare providers about your concerns.
Pale skin represents one of the most noticeable external signs of iron deficiency, resulting from reduced hemoglobin levels that give blood its characteristic red coloration. When hemoglobin decreases, the blood becomes less dense, causing the skin to lose its healthy rosy hue. This pallor appears most dramatically in areas where skin is naturally thin, such as the inner eyelids, nail beds, and the mucous membranes inside your mouth. You may also notice that your complexion looks washed out or sallow even when you feel you are getting adequate rest.
Brittle nails and hair changes commonly accompany iron deficiency, reflecting the body’s prioritization of oxygen delivery to vital organs over non-essential tissues. Your nails may become fragile, splitting or breaking more easily than usual, and may develop a spoon-shaped curvature known as koilonychia in more advanced cases. Hair may become noticeably thinner, drier, and more prone to shedding, with some individuals reporting increased hair loss during washing or brushing.
Cold hands and feet persist even in warm environments because the body redirects blood flow toward essential organs when oxygen transport becomes compromised. This reduced circulation to extremities leaves them feeling chilly and may be particularly noticeable when others around you are comfortable. In severe cases, you might experience numbness or tingling in addition to the persistent cold sensation.
Heart and Breathing Problems
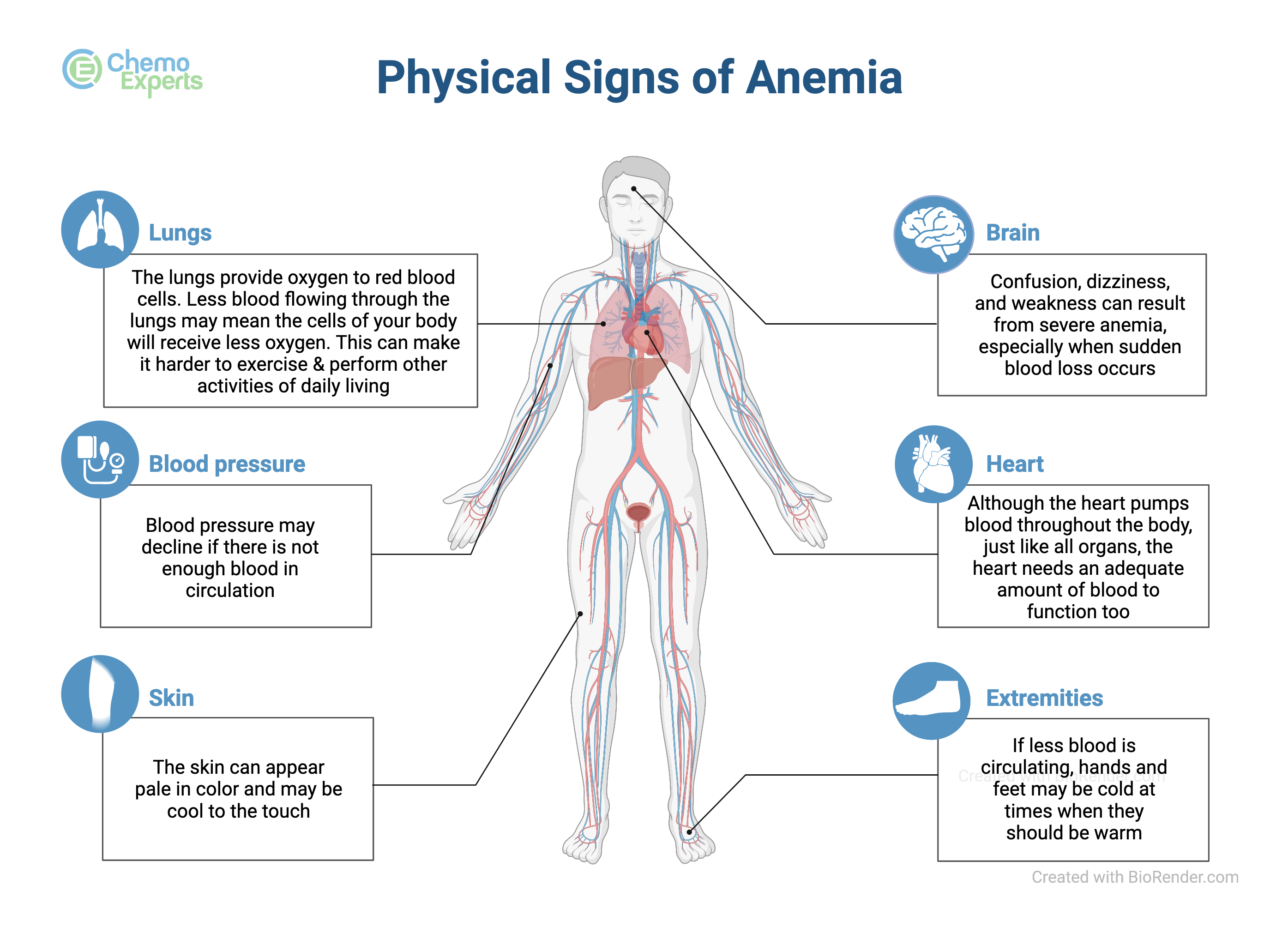
When iron deficiency remains untreated, the cardiovascular and respiratory systems work increasingly hard to compensate for reduced oxygen-carrying capacity in the blood. These compensatory mechanisms produce noticeable symptoms that indicate your body is struggling to maintain adequate oxygen delivery under stress.
Shortness of breath occurs because your lungs work to increase oxygen intake when blood cannot carry adequate supplies to tissues. You may notice this symptom during physical activities that previously caused no breathing difficulty, such as climbing stairs, walking uphill, or carrying heavy items. As deficiency worsens, breathlessness may occur during routine activities or even at rest, signaling significant compromise of your oxygen transport system.
A racing heart rate, medically termed tachycardia, develops as your heart pumps more rapidly in an attempt to deliver more oxygenated blood throughout your body. This rapid heartbeat may be particularly noticeable during exertion but can persist even when you are sitting quietly. You might feel your heart pounding in your chest or notice an irregular rhythm that seems different from your normal heartbeat pattern.
Seek immediate medical attention if you experience chest pain along with other iron deficiency symptoms, as this could indicate significant cardiac strain requiring prompt evaluation.
Brain Fog and Mental Effects
The brain consumes approximately twenty percent of the body’s oxygen supply despite representing only about two percent of total body weight, making it extremely sensitive to reductions in oxygen delivery. Iron deficiency therefore produces cognitive symptoms that many individuals find among the most frustrating and functionally limiting consequences of the condition.
Brain fog describes a cluster of mental symptoms including difficulty concentrating, memory problems, mental fatigue, and reduced mental clarity. You may find that thoughts seem sluggish, that you cannot access information and memories that previously came easily, or that maintaining focus on tasks requires unusual effort. Students may struggle with coursework that previously presented no difficulty, while professionals may find their productivity and accuracy suffering in ways that affect work performance.
These cognitive effects often persist even after other symptoms improve with treatment, suggesting that brain recovery may take longer than physical recovery. Research indicates that some cognitive functions require extended periods to return to normal, emphasizing the importance of addressing iron deficiency promptly to minimize lasting effects on mental function.
Root Causes of Deficiency
Blood loss represents the most common cause of iron deficiency in adults. For women of reproductive age, menstrual bleeding typically accounts for deficiency, with heavy periods causing particularly significant iron losses over time. Gastrointestinal blood loss causes most cases in men and postmenopausal women, occurring from conditions such as ulcers, hemorrhoids, colorectal cancer, or inflammatory bowel diseases. Because this type of blood loss often happens slowly without visible signs, it may go undetected for extended periods.
Malabsorption prevents the intestines from properly absorbing dietary iron regardless of intake adequacy. Celiac disease causes autoimmune damage to the intestinal lining that impairs nutrient absorption generally, while certain weight loss surgeries bypass anatomical regions where iron absorption primarily occurs. Individuals with these conditions may struggle to maintain adequate iron levels despite consuming appropriate foods.
Inadequate dietary intake contributes to deficiency in individuals following restrictive diets, particularly vegan and vegetarian eating patterns. Plant-based iron, called non-heme iron, absorbs less efficiently than the heme iron found in animal products. Pregnant and lactating women have increased iron requirements that may be difficult to meet through diet alone, making supplementation often necessary during these periods.
Diagnostic Testing Methods
Healthcare providers use several blood tests to diagnose iron deficiency and assess its severity. Understanding these tests helps you interpret results and participate actively in your care.
A complete blood count provides fundamental information about red blood cell size, hemoglobin concentration, and overall blood cell counts. In iron deficiency, red blood cells typically appear smaller and paler than normal under microscopic examination, a condition called microcytic hypochromic anemia. Hemoglobin levels below normal ranges confirm anemia, while the degree of reduction indicates severity.
Serum ferritin measurement reflects the body’s iron stores and provides the most sensitive indicator of early deficiency. Ferritin levels decrease before anemia develops, allowing detection of deficiency at earlier stages when intervention may be simpler. Low ferritin confirms depleted iron stores even when hemoglobin appears normal.
Additional tests may be necessary to identify underlying causes of deficiency, particularly when blood loss is not obvious. These might include tests for celiac disease, colonoscopy or other gastrointestinal imaging, or assessment of menstrual bleeding patterns. Identifying and addressing root causes prevents recurrence after initial treatment.
Treatment and Recovery Options
Addressing iron deficiency involves both restoring iron levels and resolving underlying causes. Treatment approaches vary based on deficiency severity, symptom impact, and individual circumstances.
Oral iron supplements serve as first-line treatment for most cases of iron-deficiency anemia. Ferrous sulfate, ferrous gluconate, and ferrous fumarate represent common formulations, each providing different amounts of elemental iron. Most individuals notice symptom improvement within two to three weeks of starting supplementation, though several months of treatment may be necessary to fully replenish depleted stores.
Gastrointestinal side effects including constipation, nausea, and stomach discomfort commonly accompany oral iron supplementation. Taking supplements with food can reduce these effects, though doing so slightly decreases absorption. Your healthcare provider may adjust dosages or suggest specific timing strategies to minimize discomfort while maintaining effectiveness.
Intravenous iron therapy provides an alternative for individuals who cannot tolerate oral supplements, have absorption disorders, or require rapid repletion. This approach delivers iron directly into the bloodstream, bypassing the gastrointestinal tract entirely. Intravenous iron may be particularly appropriate for patients with inflammatory bowel disease, those who have had bariatric surgery, or individuals who have not responded adequately to oral treatment.
When to Seek Medical Attention
Certain symptoms warrant prompt medical evaluation to rule out serious underlying causes and initiate appropriate treatment. Knowing when professional assessment is necessary helps you take timely action.
Persistent fatigue that does not improve with rest, particularly when accompanied by other symptoms such as pallor, shortness of breath, or unusual cravings, merits medical evaluation. These symptoms could indicate iron deficiency but might also signal other medical conditions requiring different treatments.
Multiple concurrent symptoms suggest more significant deficiency requiring professional assessment. The combination of fatigue, weakness, pale skin, shortness of breath, and cognitive difficulties points toward systemic involvement rather than simple tiredness.
Individuals with known risk factors for iron deficiency should maintain ongoing communication with healthcare providers about appropriate monitoring. Those with gastrointestinal conditions, heavy menstrual bleeding, restrictive diets, or previous deficiency benefit from regular check-ins about their iron status rather than waiting for obvious symptoms to develop.
Key Takeaways
How low iron affects the body involves multiple interconnected pathways, with the primary disruption occurring in oxygen transport to tissues throughout your system. This single effect cascades into symptoms spanning physical, cognitive, and emotional domains, making iron deficiency a condition with remarkably diverse manifestations.
Early recognition of warning signs enables timely intervention and more effective treatment. Fatigue, weakness, pale skin, shortness of breath, and cognitive difficulties collectively suggest possible deficiency that warrants medical evaluation. Understanding your personal risk factors helps you maintain appropriate vigilance about your iron status.
Treatment for iron deficiency involves both restoring iron levels and addressing underlying causes. Oral supplements work for most individuals, though intravenous therapy may be necessary for those with absorption issues or intolerance. Regardless of treatment approach, patience is essential, as full recovery requires several months to rebuild depleted stores completely.





